Presented by:

Participants:
Kaitlyn Kennard, MD, Breast Surgeon
Thaer Obaid, MD, Colorectal Surgery Specialist
Anthony Scarpaci, MD, Medical Oncologist
Eduardo Fernandez, MD, Medical Oncologist
C. Jonathan Foster, DO, Gastroenterologist
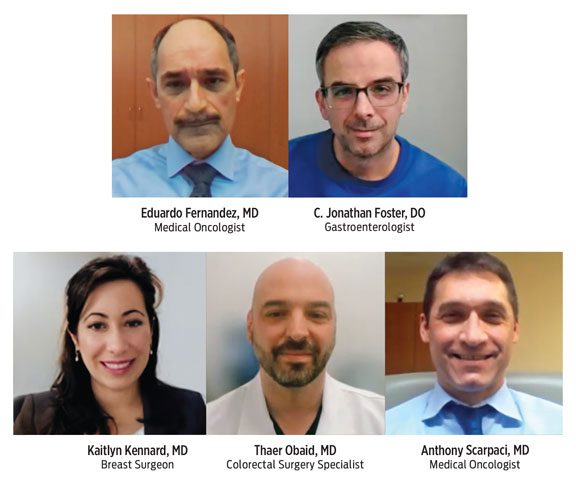 Participants are from Sidney Kimmel Cancer Center – Jefferson Health, Jefferson Cherry Hill & Washington Township Hospitals
Participants are from Sidney Kimmel Cancer Center – Jefferson Health, Jefferson Cherry Hill & Washington Township Hospitals
- For the first time ever, the ACS expects over 2 million new cancer cases in 2024.
- Incidence of 4 screenable cancers are on the rise: breast, prostate, colorectal and cervical.
- Cases of cancer in people over age 65 is declining.
- Cases of cancer in people between the ages of 50 and 64 is increasing.
- In the 1990s, colon cancer was the 4th leading cause of death for men and women under age 50. It is now the first cause of death for men under 50 and the second cause of death for women under 50.
We asked Cancer experts from Sidney Kimmel Cancer Center – Jefferson Health to talk with us about the new research and what we all should know about this serious health issue.
According to the ACS study, incidence of cancer in people over age 65 decreased. And the number of cancer cases in people between the ages of 50 and 64 increased. Why?
Part of it has to do with screening. Every time they institute a new screening strategy, you get an uptick in the incidence of cancer, but down the road it makes a difference by decreasing the incidence. That’s what we’re now seeing in the older population. There was also such a significant push to get people to stop smoking years ago, when smoking-cessation programs started. We’re seeing a decline in smoking-related cancers as well as other medical problems associated with smoking.
Dr. Eduardo Fernandez
The screening age for colon cancer is now 45 for all individuals. That’s changed within the last few years, so we’re screening earlier and picking things up earlier. Maybe someone is 40 years old and they come in with abdominal pain or even a family history of colon cancer, we do a colonoscopy and find an advanced polyp. If they hadn’t gotten their screening colonoscopy until they were 50, that most likely would have advanced to an early-stage cancer. We’re finding more advanced lesions earlier and preventing cancer later on.
Dr. C. Jonathan Foster
While we are finding more cancers in that younger population because we’re looking for more cancers, there are factors at play that we should start to consider about our lifestyle choices. There are higher incidences of obesity and sedentary lifestyles compared to other times. These are contributing factors along with other environmental exposures.
Dr. Anthony Scarpaci
For breast cancer, we are now recommending yearly mammograms starting at age 40. And for women who have dense breasts, we are recommending adding full breast screening ultrasounds, which allows us to detect more cancers earlier. For women with a high lifetime risk of breast cancer, we are often adding MRI, which we know is very sensitive and gives us the opportunity to detect breast cancers at a younger age. It’s great for patients, because it gives them many more options when we detect it earlier. That is giving us some of those earlier incidence of breast cancer for a younger population.
Dr. Kaitlyn Kennard
As a younger population is diagnosed with cancer…
For younger individuals, they often say, “I eat healthy, I don’t smoke, I exercise, I get my screening, I do everything I’m supposed to do, and this happens.” My only response is maybe if you hadn’t done that we’d be talking to you 10 years earlier, so maybe it did make an impact. Some solace, I guess, in a diagnosis that has nothing good about it.
Dr. Eduardo Fernandez
I don’t have a lot of people who think they’re too young to get cancer. Many people kind of come in with the “Why me?” question – What did I do wrong? It’s shocking for anyone, but I think there’s still a general sense that cancer can affect anyone regardless of age.
Dr. Anthony Scarpaci
I often find my younger patients are concerned about how their diagnosis is going to affect everyone else in their life – their children, their partner, their job. I remind them that they are the most important person right now and give them the analogy of being on the airplane and needing to apply your own facemask first. We will take care of them and get the whole family and their whole life through this and get them back to their normal life.
Dr. Kaitlyn Kennard
According to the ACS study, cases of colon cancer are on the rise…
For a standard individual, the age recommended for colorectal screening – where we look for polyps or the causes of a patient’s symptoms – is now 45. The majority of the time polyps are pre-cancerous lesions, so we try to remove those prior to them becoming full of cancer. The number of polyps we find will determine when a patient would be screened again. We can remove some polyps endoscopically, as well as with complex polypectomy techniques. If we can’t remove a polyp endoscopically, we refer for a surgical removal.
Dr. C. Jonathan Foster
There are 3 steps in managing colon cancer. The first one is the diagnosis, when we do the colonoscopy, take a biopsy and put a special mark at the location of the mass. The second step is staging, when we obtain blood work and a CT scan to see if the cancer has already spread throughout the body. The third step is surgery – called an oncological resection – where we remove that section of the bowel, surrounding lymph nodes and the vascular supply. Then that specimen will be sent to pathology to identify if the lymph nodes are involved or not.
Dr. Thaer Obaid
In addition to the rise in colon cancers, the ACS Study also showed that cases of breast cancer are on the rise, and yet some people still delay their colonoscopy or mammogram…
I tell patients it’s usually not a night out in Las Vegas, but it’s a procedure that’s going to prevent any future risk for you. Colon cancer is so easily preventable because of screenings. But if patients are really set against it, there are other options. We can use DNA stool tests to determine if the patient has an increased risk of having an advanced adenoma. If that is positive, then they would need a colonoscopy. There is also now a CT colonography, so basically a patient can have a CAT scan to determine if there’s any polyps or lesions throughout their colon. There are non-invasive options now which is great, and that’s definitely increased our screening ability for patients who are not willing to undergo colonoscopy.
Dr. C. Jonathan Foster
Many women are getting mammograms, but the patients I see delaying their mammograms are sometimes the ones who are at greatest risk. They’ve seen a family member diagnosed with breast cancer, and that fear can be paralyzing. So sometimes the women we need to capture most are the ones who are not getting their screening mammograms. As a community, if we know friends or family members who may be at risk, don’t be afraid to say, “Hey, have you started your mammogram?” If the answer is no, be that friend who tells them this is something that’s really important and help them start the process. Be open to that conversation. Because once they start the process, it’s much easier. It’s that initial mammogram that can be really tough for women.
Dr. Kaitlyn Kennard
What people don’t know about cancer…
There’s a perception that cancer is one type of disease, and it goes to different parts of the body. One of the challenges we have is trying to explain how these cancers are biologically different. Breast cancer is different than colon cancer which is different than lung cancer. And treatment options differ because the biology is different. It’s not just one disease. There is also a prevailing sentiment that cancer equals death. But there are many treatable and curable forms of cancer. Cancer treatment is different than what it was several years ago. In many situations, there are curable cancers and if it’s not curable, there are treatment options to help people have a better quality of life for a longer period of time.
Dr. Anthony Scarpaci
People have the perception that cancer is some unbeatable foe. When I look at a patient with advanced cancer, yes, the inevitability is we may not be able to cure their disease, but that’s not a foe you can’t beat in the sense of how does that impact your mental health? Your willingness to live? Your relationship with other people? Your outlook on life? So when people say, once you have cancer, you’re done, I think you need to separate the physical from the mental and spiritual. Those things are pretty critical in dispelling the myth that you have no chance.
Dr. Eduardo Fernandez
Some people think there is only one best treatment option for them. What’s really exciting about breast cancer treatment is there are many options, and they’re tailored based on the patient’s tumor biology as well as the patient. I see my role as helping each patient select the treatment option that’s best for them personally and best for their cancer.
Dr. Kaitlyn Kennard
With the help of biotechnology advancement, subspecialization and strict screening protocols, we’re not only able to treat cancer, we’re able to prevent it early. So early detection and prevention plays a key role in the survivability of cancer.
Dr. Thaer Obaid
The ACS study cited treatment advancements as one reason for the downward trend in the risk of dying from cancer. Cancer research continues to show promise…
People should be optimistic about the future of cancer research. The pancreatic cancer survival for stage 4 has gone up from about 8% to 12%.
Dr. C. Jonathan Foster
In breast cancer research, targeted therapies are what’s most exciting right now. We can target patients based on their subtype of breast cancer, and by using more targeted chemotherapies we often can remove less lymph nodes in the axillae which decreases a woman’s risk of lipedema. We can also provide more precise radiation, which has fewer side effects, which is really exciting for our patients.
Dr. Kaitlyn Kennard
We always hope for the big jump when there’s a major treatment that changes things significantly, but it’s typically incremental. If we go back to when I started my career, which wasn’t too long ago, we didn’t have as many options as we do now. Cancer research is a very hopeful thing for people to hear about. People have a larger healthcare literacy than they used to, so they’re usually interested in understanding what’s coming down the road.
Dr. Anthony Scarpaci
What’s made a change in how we treat patients is cancer genomics, where researchers look into the driving mechanisms of cancer beyond the scope of what traditionally has been our treatment. We’ve learned there is not one treatment that fits all diseases, and that’s where I think we’re headed with precision medicine. Patients have been given a lot more options, and we’re seeing much better probability of long-term survivals.
Dr. Eduardo Fernandez
What sets Jefferson’s cancer program apart…
The benefit of coming to Jefferson is we have multiple subspecialties working together. Every cancer patient is different, and the treatment is usually tailored to each individual patient. So the ability to come to a center where we have all subspecialties working together has an impact on the outcome. We have direct communications between the multiple teams, and we have our tumor boards, where we discuss every patient individually to come up with one agreed-upon plan.
Dr. Thaer Obaid
In the scope of understanding where cancer patients are with their diagnosis, the most important element is seeing the patient as quickly as possible. If any of my colleagues sends me a message about a patient, I’ll immediately work on somehow fitting that patient in, typically within a day or two. I’ve been on the other side, where I’ve had a family member with a new diagnosis of cancer and scheduling that initial visit was one of the most important aspects of the whole process. We all take our computers on vacation, we all have our cell phones on. It’s very helpful for patients to know they can be seen very quickly here. It means the world when somebody cares.
Dr. Eduardo Fernandez
The Sidney Kimmel Cancer Center is an NCI-designated center. The advantage we have is that we’re a very large enterprise now, so we have specialization and resources throughout the metro area. It’s not just our local group of physicians and colleagues – we can communicate with a larger network to have access to the latest technologies and clinical trials for our patients.
Dr. Anthony Scarpaci
Jefferson’s tumor board…
The tumor board is basically a meeting where the oncologists, surgeons, GI specialists, radiation and genetics specialists, and the cancer navigator all meet, and we present patients to formulate a plan for the management of their cancer. We meet bi-weekly for about an hour to review all the data and then decide on treatment.
Dr. Thaer Obaid
You can think of the tumor board as a free second opinion from every specialist involved in your care. Everyone who assists the patient is there to hear what that patient needs and then provide input as to what the next steps are in their care.
Dr. Eduardo Fernandez
Who can get cancer…
In terms of colorectal cancer, genetics plays an important role. 10-20% of newly diagnosed cancers are related to underlying hereditary disease. There are also environmental factors: obesity, smoking, high fat and red meat intake, and poor access to healthcare all play a part in increasing the risk of colorectal cancer.
Dr. Thaer Obaid
Anybody.
Dr. Anthony Scarpaci
One in 8 women get breast cancer – 12 1/2% of all women. And many breast cancer patients don’t have any family history, they don’t have any genetic mutation. Breast cancer is something that, unfortunately, really doesn’t discriminate based on age, race, gender or socioeconomic status.
Dr. Kaitlyn Kennard
The ACS Study noted that obesity remains a cause of many cancers. Could the increased use of new weight loss drugs cause a decline in cancer cases?
No. While the medications do cause weight loss, they are not really causing behavioral changes or lifestyle changes, and that’s really the larger picture.
Dr. Anthony Scarpaci
Obesity is just one factor in the development of cancer. What people look for when they see these medications is a physical transformation of their body, not a behavioral change. They may eat less, but they’re not eating the right foods, they’re not exercising, their stress levels are the same. Those are really the integral components of why obesity compounds the risk of developing cancer.
Dr. Eduardo Fernandez
The other issue with those medications is that once you stop taking them, you have obesity again. That connection between obesity and cancer is complex. It’s hormonal changes throughout the body, and by losing weight, you’re not necessarily changing your diabetes risk, your insulin level or your lectin level or the different hormonal changes that are caused by obesity.
Dr. Thaer Obaid
I’m going to play devil’s advocate. Obesity is a risk factor for breast cancer and any other cancer, so if there is a tool in the toolbox to help patients get on a path to a more healthy lifestyle, with them exercising and eating more healthy, I think it’s great. But patients should understand that this is something that’s going to be a jump start, something to correct the trajectory. The help doesn’t come from just this medication but a whole suite of things that need to be done. I don’t personally prescribe those medications, but if it’s something that gets patients headed in the right direction, that could lead to an initial 20-pound weight loss and gets them into a lower risk category, potentially they can do better with the outcomes.
Dr. Kaitlyn Kennard
The ACS study noted an increase in breast cancer, yet the prognosis is good…
For all stages of breast cancer, the overall survival rate is over 91%. However, for early breast cancers, stage 1, which many of our breast cancers are being detected at this stage with screening mammography, the 5-year overall survival is over 99%. It’s really amazing the outcomes and survival rates we see with these patients.
Dr. Kaitlyn Kennard
Preventing breast cancer…
There are many risk factors for breast cancer. Some are modifiable, so things we can change, and some are non-modifiable, such as our family history or our genetics. But there are many things we can do to decrease our risk of breast cancer. They include decreasing alcohol intake – alcohol intake greater than 3 drinks per week for women has shown to increase our risk of breast cancer. Another is maintaining a healthy lifestyle and healthy weight – obesity is linked to an increased risk of breast cancer. Another risk is delaying pregnancy ’til later in life – having your first child over age 30 does increase our lifetime risk of breast cancer. But breastfeeding decreases our incidence of breast cancer, so for women who do choose to start a family later in life, I encourage them to try breastfeeding to help counteract that increased risk.
Dr. Kaitlyn Kennard
What they like about the work they do…
I like the intensity. It’s the one field of medicine where you create a very trusting mutual relationship – that is really gratifying. There is a lot of science and technical aspects of what we do, but the humanistic aspect of cancer care is what drives me to put what I need or want to do aside, and be there for patients. Because I know I’d like somebody to be there for me.
Dr. Eduardo Fernandez
We do this to help people, and we get to help in very unique ways. We get to help when someone is sick. We get to help when we have to talk about bad news. You don’t usually think about that as a way of helping someone, but that’s a really important aspect of our job, when we have to help someone and their family through a very difficult situation.
Dr. Anthony Scarpaci
I like the humanistic aspect and I like the technical aspect – being able to diagnose and then send a patient to one of my colleagues who will help treat this new disease.
Dr. C. Jonathan Foster
I really love being there for women at a difficult time. No one expects or plans for a breast cancer diagnosis. Being able to tell women they’re going to do well, and we’re going to get through this together is really rewarding. I see my job as helping them select a treatment option they’re going to be happy with 5, 10 and 20 years down the road, when breast cancer is just something in their rearview mirror.
Dr. Kaitlyn Kennard
This is a very dynamic field. There’s always new research, new technology, new treatment options, so you always have to stay updated to offer the patient the best treatment options. There are no two patients who are 100% the same. Being able to tailor treatments to each patient individually keeps us challenged.
Dr. Thaer Obaid
Lessons from their cancer patients…
I’ve witnessed the resilience of being a human being. You go from fear and dread to understanding and acceptance. You grieve. But the most fascinating aspect of every individual we treat is that everybody is different. Some get through it with stars, and some don’t. It really is a life lesson.
Dr. Eduardo Fernandez
I’m absolutely amazed at the human spirit. It’s very rare for a patient to say, “Boy, I wish I had bought this thing or I had worked more.” Often it comes down to discussions about wanting more time with a significant other or family or friends. That’s what I’ve learned – what’s truly important.
Dr. Anthony Scarpaci
I’ve learned the importance of relationships. We have a relationship with the patient as part of their breast cancer team. But they also have what I call their team outside the hospital – their family and friends, and that’s really who supports them through their journey. It has taught me to value the importance of relationships both in my work and outside of the hospital.
Dr. Kaitlyn Kennard
A lot of the cancers we find can be fairly progressed, stage 3 or stage 4, but patients are fighters. They want to keep going for their family and their friends, and we do what we can to keep their quality of life and keep them going. So I’ve learned how resilient our patients can be.
Dr. C. Jonathan Foster
With every new diagnosis of cancer, no matter what the stage is, the first thing the patient thinks about is how many more days, months or years they have to live. At that moment, they’re looking at themselves like maybe I’m not going to be here in a year, and that changes everything. It puts everything into perspective. I have found it to be a very humbling experience. They just sort of appreciate what’s really important in life, which is family and friends and health.
Dr. Thaer Obaid