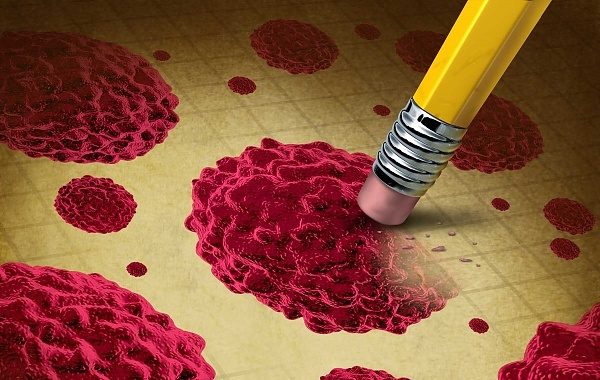
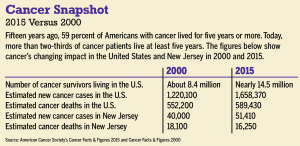
Cancer is the second leading cause of death in the United States (right behind heart disease), but the disease is losing its stronghold. Over the past 15 years, advancements have improved quality of life for millions of patients and boosted life expectancy for millions more. Today, a record number of cancer survivors are alive: nearly 14.5 million Americans.
“Cancer death rates in the U.S. have been declining 20 percent over the last 15 to 20 years,” says Stephen Zrada, MD, chief of medical oncology at Virtua. “Cancer survivorship is becoming a hot topic in oncology and medicine in general, because there are an unprecedented number of cancer survivors.”
Today, 68 percent of people with cancer live five years or more, compared to 59 percent in 2000 and 49 percent in 1975, according to the American Cancer Society.
“Cancer has come out as a disease that you can acknowledge having,” says Generosa Grana, MD, director of the MD Anderson Cancer Center at Cooper and head of the division of hematology and oncology at Cooper University Health Care. “It’s not a death sentence.”
Dedicated researchers and oncologists – with the help of countless cancer patients who participated in clinical trials – have discovered, created and implemented the use of powerful weapons in the fight against cancer. Here are some of the most notable achievements from the past 15 years:
 Changes to chemotherapy
Changes to chemotherapy
In 2015, this is not your mother’s chemotherapy. Decades ago, chemotherapy drugs were more powerful than they needed to be, so patients felt nauseous after every treatment.
“Previously, most anti-cancer agents were basically poison,” says Randy Strich, PhD, molecular biologist at the Rowan University Graduate School for Biomedical Sciences. Strich has conducted cancer research for the last 23 years. “They’d give the patient enough poison to kill the tumor, without killing the patient.”
Today, doctors have better chemotherapy options for patients, which include superior anti-nausea treatments and a variety of drugs that work together to combat the cancer.
“Instead of giving a large dose of a particular type of agent, they give you a cocktail of different compounds,” Strich says. “You’re damaging the tumor, and you don’t have as much drug resistance.”
Targeting specific cancers
One of the biggest changes in cancer treatment over the past 15 years has been targeted therapy for specific types of cancer. Researchers have pinpointed the causes of several cancers and discovered new medications that target those problems. The drugs attack tumor cells without harming patients’ healthy cells.
“Once you understand the pathways that go awry and cause a tumor to form, you can identify the proteins along those pathways,” Strich says. “By knocking that activity down, you’re specifically affecting the tumor and not other cells.”
One of the earliest targeted therapies was Gleevec, a drug that was approved to treat chronic myeloid leukemia in 2001. “This drug was considered one of the first targeted therapies that revolutionized how we treat that disease – taking a pill instead of undergoing a bone marrow transplant,” Virtua’s Zrada says.
Another important targeted therapy drug, Herceptin, was approved in 2005 for women who have HER2-positive breast cancer. “It’s not cookbook medicine, where one regimen is good for all,” Grana says. “Different subgroups behave differently, more or less aggressively, and can be treated in different ways. The treatments are specialized.”
Targeted therapies have helped doctors personalize treatments for their patients to get optimal results for more than a dozen types of cancer.
“These new treatments are allowing us to provide precision medication,” Zrada says. “If a person doesn’t have a particular mutation, you’re not going to use the drugs, but if they do, these targeted therapies will work better. You’re sparing some patients drugs that have very little chance of working and maximizing other patients’ chances of responding to a drug.”
Assessing whether treatments are necessary
Technology has helped doctors realize that chemotherapy or radiation isn’t always necessary.
Some breast cancer patients can safely avoid chemotherapy after surgery if gene analysis of their tumor cells shows it won’t be beneficial.
“A gene assessment of the tumor helps you predict the behavior of the cancer to give a better idea whether it is high-risk or low-risk, whether someone needs chemotherapy or not,” Grana says. “In the past, women with tumors one centimeter or larger – the size of a chick pea – were recommended chemotherapy and hormone therapy. Now some can avoid it and just get hormone therapy.”
For rectal cancer patients, MRI images can help doctors determine how advanced the disease is and whether patients will need radiation.
“Historically, you get radiation, chemotherapy, surgery,” Goodworth says. “Then, if the disease comes back, you can’t re-radiate the same area. We’ve been able to determine the stage of the disease with MRI. If the disease is stage 1 or 2, the patient can forgo radiation. All the trials have shown it doesn’t affect long-term outcome. In the future, if they need radiation in the pelvis, they can get it.”
Vaccines against cancer
Some cancers are caused by viruses. Cervical cancer, for instance, is caused by the human papillomavirus (HPV). In 2006, the FDA approved the Gardasil vaccine, which protects against the HPV strains that cause about 70 percent of cervical cancers. It was the first vaccine approved to prevent cancer. “That’s considered a breakthrough,” Zrada says. “It’s a growing field.”
Immunotherapy
In the past three years, researchers have been making strides in the field of immunotherapy, which uses the body’s immune system to fight cancer. “Think of tumor cells as a foreign infectious agent,” Strich says. “You look for proteins in the tumor to be a target for the immune system. You can change your immune response pathways so they see tumor cells as foreign bodies, and your own immune system will be geared to take out the tumor cells.”
Advanced lung cancer screening
More people die from lung cancer than any other form of the disease. Historically, most lung cancer patients have been diagnosed at stage 4, when the disease has already spread to other parts of the body and treatment options are limited.
This began changing in 2013, when the American Cancer Society and the U.S. Preventive Services Task Force recommended that doctors offer certain high-risk patients a low-dose CT scan to screen for lung cancer. This non-invasive screening tool can identify cancer at an earlier, more treatable stage than a chest X-ray.
“A person who has a significant smoking history in an appropriate age range – 55 to 80 – would come in and get a CT scan of the chest,” says radiologist Gregory Goodworth, MD, head of body imaging at South Jersey Radiology Associates.
This new screening tool can reduce lung cancer deaths by up to 20 percent, compared to chest X-rays. “This helps people catch stage 1, when a cure is possible, instead of stage 4,” Goodworth says. “You find the disease when it starts, rather than when they say, ‘I’m short of breath, I’m coughing up blood.’”
Virtual colonoscopy
The best screening tool against colon cancer is colonoscopy, which is recommended every 10 years for people age 50 or older. If a pre-cancerous polyp is discovered, the doctor can remove it during the procedure.
“In terms of detection, nothing is better than routine screening,” Goodworth says. “Colon cancer is one of the easiest to catch early and prevent.”
But some patients can’t undergo a traditional colonoscopy. They may have colons that curve or narrow in such a way that doctors can’t insert the necessary equipment. Other patients may have endured so many surgical procedures in the past, their doctors recommend against another invasive procedure. And some take blood thinners, which can cause complications during or after colonoscopy.
Fortunately, these patients have had another screening tool available to them for the past decade: virtual colonoscopy. Doctors use a CT scan to examine a patient’s intestines. The patient’s bowel is inflated with air and the doctor takes pictures, which a computer turns into a 3-D image of the colon.
“The big difference is if you find something, you can’t do anything about it at that time,” Goodworth says. “The advantage is there are no complications.”
Powerful MRI catches prostate cancer
Getting tested for prostate cancer can make men feel squeamish, especially when you consider that until recently, anyone who needed an MRI of the prostate gland needed a special device (an endorectal coil) placed into the rectum for the duration of the procedure. “The compliance rate was very, very low,” Goodworth says.
Five years ago, a more powerful machine, called 3 Tesla (3T) MRI, began changing the way that doctors can diagnose prostate cancer. “The magnet is so powerful, you no longer need an endorectal coil,” Goodworth says. “The compliance rate is essentially 100 percent. The quality of the pictures allows me to pinpoint where in the prostate the clinically significant tumor is located.”
Assessing risk for breast cancer
In 2013, actress Angelina Jolie made headlines for having both of her breasts removed when she learned she carried a mutation of the breast cancer gene BRCA1. Since then, doctors have been meeting with an increased number of patients concerned about their breast cancer risk.
“In medical oncology, we call it the Angelina effect,” Grana says. “There’s been an increased number of women coming in and asking for additional services, based on that.”
When a woman is identified as high-risk, whether or not she has a mutation of BRCA1 or BRCA2, she’s offered more frequent breast screenings, including digital mammography plus MRI. Her doctor may discuss other options, including drugs, to lower her cancer risk.
“They should not assume if you have a family history that surgery is the only option,” Grana says. “Many women are never ready to do surgery. Now we have drugs we can give to high-risk women to lower risk, like tamoxifen and raloxifene. And we can discuss what to do about risk in terms of modifying lifestyle factors. Exercise may be protective. Alcohol can be harmful.”

 Changes to chemotherapy
Changes to chemotherapy