Kayleigh Summers was screaming. That’s not so unusual for a woman who is 10 centimeters dilated in a hospital delivery room. But this was different.
“I started yelling, ‘Something is wrong. Something is wrong with my heart,’” says Summers, a Voorhees native. That’s when her heart stopped beating. Just moments before, the nurse was smiling, asking if she and her husband were excited to meet their baby. Then the nurse was calling a Code Blue for Room 231.
Doctors rushed her to the OR, and 6 minutes later, her son, Callahan, was born. While half of the room focused on resuscitating him, the other half worked on Summers. She was down for 9 minutes before she was revived. Then she started bleeding uncontrollably. After receiving 143 units of blood (the average person holds 10 units of blood in their body), she coded again.
Doctors put Summers on the highest form of life support while working to stabilize her. She underwent a hysterectomy to stop the bleeding. She was given a heart pump to maintain blood flow. Two days later, Summers finally came off life support.
Or, at least, all of this is the story she was told. She remembers getting her nails done days before the delivery. The next thing she knew, she was in the Cardiothoracic ICU with her OB/GYN and anesthesiologist sitting on either side of her bed, holding her hands. Her son wasn’t there, and after more than an hour of listening to the events of the last few days, she understood why.
“I remember wanting all of the information,” says Summers. “I just kept thinking, ‘Please, don’t stop talking.’”
Summers suffered from an amniotic fluid embolism, an extremely rare and often fatal occurrence that happens without warning in only 1 in 50,000 births. Summers and her son Callahan, now 2, are both happy and healthy. But the experience still lingers. She started sharing her story publicly – first on Instagram, then later on TikTok under the handle @thebirthtrauma_mama – in January 2020.
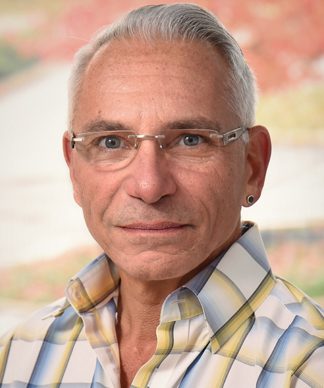
Anthony Salerno, MD
“I wanted to raise awareness for my and other women’s experiences,” she says. As rare as her condition was, her birth experience is more common than many soon-to-be parents want to believe. Up to 45% of new mothers have experienced birth trauma, according to a recent study published in the National Library of Medicine.
“When you tell people you’re an obstetrician, they think, ‘Oh, what a happy field. How wonderful,’” says Anthony Salerno, MD, acting chair of the Department of Obstetrics and Gynecology at Rowan University School of Osteopathic Medicine. “And it is 99% of the time. But 1% of the time, it can be devastating.”
To a doctor, a “traumatic” birth would be anything that unexpectedly causes harm to either the mother or baby. Something like a vaginal or perineal tear after delivering a 9 lbs baby is not unexpected, he says, but a 4th-degree tear from the vagina straight to the rectal sphincter certainly is. “A traumatic birth for a mother would be anything resulting in an excessive loss of blood, called a postpartum hemorrhage complication, which is the leading cause of maternal mortality,” says Salerno.

Theresa Adeliyi, MD
For a baby, he says, a traumatic birth would be anything that causes injuries, such as a thumb injury, or if the shoulders get impacted, which can cause cervical nerve damage. Anything involving forceps or a vacuum delivery would be traumatic for them both.
In terms of preparing ahead of time, there’s a happy medium between coming to the hospital unaware and completely freaking yourself out, he says.
“You want an informed patient, not a panicked patient,” he adds. “It’s our job to refocus and realign the expectation. But in between coming to the doctor’s office, patients are talking to their friends, family members, Google and getting a whole host of information that is sometimes helpful and sometimes extremely misleading.”
Making a birth plan can help prepare for the big day, especially if something goes wrong, says Theresa Adeliyi, MD, a provider at Virtua Center for Women in Voorhees.
“As physicians, sometimes we roll our eyes at birth plans because something like that will never go according to plan. But what this does is open up a dialog,” she says. “I review a plan line by line to tell them if these are things we already do or to say no, this doesn’t make sense.”
That also creates this opportunity to correct misinformation, she says, and to help partners get involved.
“There are situations where a patient is tired,” Adeliyi says. “She’s groggy. She can’t remember the conversations that she had with a doctor. In those situations, partners can be their advocates.”
Kayleigh & Steve Summers go home with Callahan
The effects of a traumatic birth can linger long after leaving the delivery room, leading to postpartum depression and post-traumatic stress disorder in addition to physical complications.
“Depression is already high for patients after the delivery,” says Adeliyi. “But when you have a traumatic experience during birth, it increases the risk of depression by at least 2 times.”
That was Summers’ experience. On top of recovering from her physical injuries and trauma, that instant mother-son connection wasn’t there.
“I don’t remember having a sense of being overjoyed,” she says. “I was just kind of like, ‘Are you sure this is my baby?’ Which is such a terrible feeling to have.”
Her husband Steve was incredibly supportive, she says, but it affected him too.
“It was traumatizing for him to see me go into cardiac arrest with our child inside me,” she says. “He had to sign consent forms. He gave consent for the hysterectomy, which is an awful position to put him in. When he met our son, he started hysterically crying, just like, ‘Oh God, I’m going to have to do this all by myself.’”
Summers is a therapist, and she knew she and her husband needed therapy as soon as possible. “When I left the hospital, I cried tears of joy and gratitude that I was alive. But in the back of my head, I knew this was really going to mess me up.”
Summers says that post-traumatic stress disorder and postpartum depression have been taboo subjects in the past, but that’s starting to change. She’s found an eager audience on social media who is ready to hear her story – and share their own. It can be hard sometimes, she says, but it’s an important conversation to have.
“I am so lucky and grateful to have lived through this, but at the same time, I’m also sad and angry that this happened to me,” says Summers. “I still grieve what I thought my birth experience would be. I wasn’t even technically alive when my baby was born. And now I’ll never have another pregnancy. I’ll grieve that for the rest of my life. I’m so grateful for where I am today, but that doesn’t go away.”














