Since guidelines for mammography were lowered to age 40 for annual screenings, more women are being diagnosed with early-stage breast cancer. That’s actually a good thing for the outcomes of most of those women. (The earlier the breast cancer is found, the more likely the patient will fully recover.) But it also means you probably know someone who has been diagnosed with the disease. You may even know more than one person. We sat down with South Jersey breast cancer experts to find out what we all should know about the disease, whether we’re the patient, family member or friend.
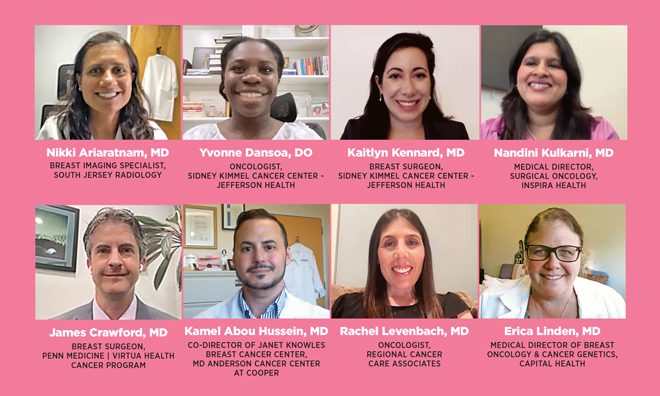
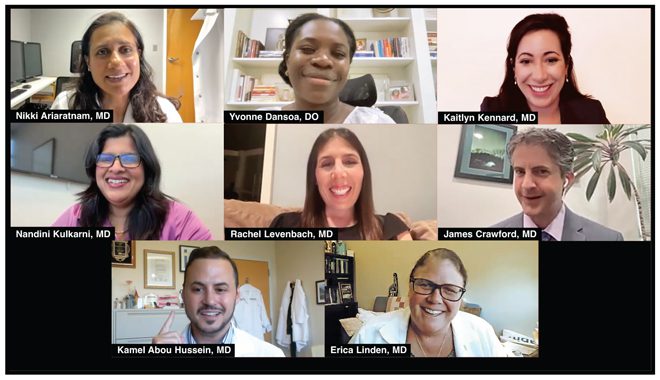
Participants:
Nikki Ariaratnam, MD Breast Imaging Specialist, South Jersey Radiology
Yvonne Dansoa, DO Oncologist, Sidney Kimmel Cancer Center – Jefferson Health
Kaitlyn Kennard, MD Breast Surgeon, Sidney Kimmel Cancer Center – Jefferson Health
Nandini Kulkarni, MD Medical Director, Surgical Oncology, Inspira Health
James Crawford, MD Breast Surgeon, Penn Medicine | Virtua Health Cancer Program
Kamel Abou Hussein, MD Co-Director of Janet Knowles Breast Cancer Center, MD Anderson Cancer Center at Cooper
Rachel Levenbach, MD Oncologist, Regional Cancer Care Associates
Erica Linden, MD Medical Director of Breast Oncology & Cancer Genetics, Capital Health
Breast cancer myths
There’s a belief that if we remove the breasts completely, all problems will be solved. I have patients who come to me with small cancers that were diagnosed early, and they’re like: Just remove both my breasts. But that’s not always the gold standard treatment. You have to tailor the treatment to the unique set of circumstances of each patient.
Dr. Nandini Kulkarni
There’s always concern about screening mammography and that it’s a radiation test to detect cancer. But the amount of radiation is minuscule. It’s actually less than the background amount of radiation we get from living in New Jersey. If you’re avoiding mammography because you’re worried about radiation, you’re missing the point. Finding breast cancer early is so much more important than the minuscule amount of radiation you’re going to get.
Dr. Nikki Ariaratnam
One myth is there is only one right treatment for breast cancer. There are actually a lot of options, which is really great for patients, but it also can be difficult, because they want to know what the one right treatment is. We look at the type of breast cancer they have and match that to the patient and their lifestyle and their desires. So the answer is, there are a lot of right treatments for breast cancer.
Dr. Kaitlyn Kennard
I’m always a big advocate of trying to dispel the myth that men don’t get breast cancer. Men absolutely get breast cancer, about 1% of breast cancers in the U.S. are male breast cancer. I advise men that if they feel a hard, firm mass behind the nipple or close to the nipple, pay attention to that. Tell your doctor.
Dr. James Crawford
People hear chemotherapy and they think, I’m going to be sick, I’m going to be home all the time, I’m going to lose a lot of weight, I won’t be able to function. But that is not the case. We have really good supportive care for patients getting chemotherapy right now. I have patients who are on chemotherapy and still continue to work through their cancer treatments.
Dr. Yvonne Dansoa
A lot of patients have this impression this diagnosis is a death sentence. Maybe years ago the treatments were harsh and quite limited. But today it’s a very, very different story – we are seeing a significant improvement in what the life of a breast cancer patient is after they are diagnosed. We’ve seen a revolution in the therapeutics that are available for treatment of breast cancer and that has led to excellent responses.
Dr. Kamel Abou Hussein
Sometimes women think if they get bilateral mastectomy, they won’t need any additional treatment or their breast cancer won’t come back. That should be discussed when they’re talking to their breast surgeon and medical oncologist. If you decide to get bilateral mastectomy, you should know the pros and cons.
Dr. Rachel Levenbach
One myth about breast cancer is that all breast cancer is inherited. Many people think that since they don’t have a relative with breast cancer, they’re not at risk for breast cancer. The number one reason people are at risk for breast cancer is age, and the second is being female. If you are getting older and you’re female, your risk for breast cancer is increasing.
Dr. Erica Linden
A patient’s first visit
I always tell patients at our initial visit that whatever I say today we are going to talk about numerous times. They may not grasp a lot of the information the first time we visit each other, but then it kind of clicks, and as the visits go on, they’re asking more questions. They’re understanding more. I think a lot of the anxiety is caused by not knowing what the future holds.
Dr. Rachel Levenbach
Typically the breast surgeon is the first doctor they’re going to actually talk to about this new diagnosis. So a lot of time is spent helping them to better understand what this new diagnosis is and more specifically, what it means for them. Most patients come in thinking this is the end essentially, or that the end is getting close. I’d say the majority of visits are actually very positive from the patient perspective. They get to realize this is a very manageable and potentially curable disease.
Dr. James Crawford
It’s a very emotionally charged visit, and that’s why we always schedule enough time so the patient never feels rushed and we have enough time to answer their questions. A visit with me for a first discussion is booked for about an hour, and I have been known to exceed that time limit sometimes, if necessary. They may break down during our discussion, just from finally coming to the realization of what they’re about to enter. I try to make them feel this is a safe space to express how they are feeling throughout their journey.
Dr. Nandini Kulkarni
My first visit with the patient is all about name it, stage it, treat it. I go through what kind of cancer they have. What does that mean? What stage is it? What is the extent of disease, and how do we treat it? I’m really looking at what is the roadmap of the next year look like. I take notes on the pathology report during our discussion, and I hand that to the patient to take home. Because often, it’s a blur for them. I want them to know this is the start of a discussion. It starts here. It doesn’t end here.
Dr. Kaitlyn Kennard
As a breast radiologist, my job is to do the biopsy when the patients are unaware of the diagnosis. My interaction with the patient is to get to know them a little bit, make them feel comfortable and make them feel at ease. I always tell patients that the microscope tells us everything, so nothing is certain until we get those results back. If the results are positive, I call the patient. Giving them that result is always difficult, but it helps that I’ve met the patient and know a little bit about them. I try to put it in the best light possible – breast cancer is immensely treatable today, so it’s just getting them to the next step, which is to see the breast specialist.
Dr. Nikki Ariaratnam
Does breast cancer always mean a mastectomy
Every breast cancer is different, and the beauty of today’s medicine is we have treatment options. We review all treatment strategies with a patient, walk them through the options, and educate them so we really are able to fine tune and tailor their treatment to what fits best for them. How much are they involved in that decision? 100%.
Dr. James Crawford
For some people, their initial response to breast cancer is just get rid of the breast, and that may be the right decision for some people, but that may be more surgery than one needs. If somebody has a dangerous breast cancer that’s aggressive and could potentially spread, then we have to say, hold on, we want to protect and treat your whole body, treat you, not just the breast. That’s one reason why we might put the brakes on going right to mastectomy. A patient might also have other medical problems, like maybe diabetes or heart disease, and they may not heal as well, so a smaller surgery may be more beneficial. This all has to be tailored to each individual patient’s cancer biology, their other medical issues and timing.
Dr. Erica Linden
Recent advancements
Breast tomosynthesis is about a little over a decade old now, but that’s essentially when we started using 3D mammography, or thin slice mammography, to help uncover architectural distortions. It helps us target smaller and smaller lesions. I just did a biopsy under tomosynthesis guidance, where I found a two millimeter breast cancer that I could not find under ultrasound. That was really incredible, because that didn’t used to happen.
Dr. Nikki Ariaratnam
I think the “less is more” approach that breast surgery has taken over the last few years is the hallmark of advancement in breast cancer treatment. It went from removing the entire breast to lumpectomy, where you can remove small areas of tissue and maintain the patient’s shape and feel of the breast.
Dr. Nandini Kulkarni
The role of immunotherapy and using your body’s own immune system to fight the cancer has been a great advancement. Another advancement is the use of targeted therapy. We have a lot of ways to find what makes a patient’s breast cancer different than others, and then we have targeted therapies that will specifically target their type. Today, the majority of patients with early-stage breast cancers are cured of their disease, and even with later-stage breast cancers, patients are living much longer and having better quality of life.
Dr. Rachel Levenbach
One great advancement has been in reconstructive options. For women who choose to have a mastectomy, we can basically reconstruct the breast during their index surgery. So at the time of their mastectomy, we can go direct to implant – the plastic surgeon comes in right behind us and places the implant. Some women choose to do tissue-based reconstruction, where tissue from their belly is moved up to the breast as their final breast reconstruction. So when women say they want breast reconstruction, there’s a great host of options, and some can all be done in one surgery.
Dr. Kaitlyn Kennard
I would say the biggest advancement is our ability to offer a much wider array of surgery, as well as to essentially downgrade some of our surgeries. Gone are the days where every patient gets a mastectomy. We are able to offer lumpectomies. We don’t have to necessarily remove all of the lymph nodes in the armpit in every case, like we used to. We can individualize treatment and allow for much better treatment of each patient’s cancer.
Dr. James Crawford
In the past, almost all patients with invasive breast
cancer were getting chemotherapy. But then the Oncotype DX score was introduced, which tells us that not all patients with hormone receptor positive breast cancers need chemotherapy, even when they have lymph nodes involved. Usually just anti-estrogen therapy alone is enough to decrease their risk of breast cancer recurrence. Having invasive breast cancer, even with up to three lymph nodes involved, does not necessarily mean you need chemotherapy. That has been a huge advantage for breast cancer care.
Dr. Yvonne Dansoa
Detecting breast cancer
Mammograms are the best chance we have for screening the entire general population from the age of 40 onwards, once a year, every year, for small breast cancers. It is the best way to detect the smallest type of breast cancer, which is called DCIS, which usually presents as tiny, micro-calcifications, which look like little dots of white sand on the mammogram. But mammograms do have some deficits: When patients have dense breast tissue, that can mask or hide breast masses. In those cases, breast ultrasound may be useful. That is a non-radiation technique that uses sound waves to look through the breast tissue to try and figure out, is this dense breast tissue or a mass or cyst?
Dr. Nikki Ariaratnam
Mammograms are the gold standard as a screening tool – very low risk, and for the most part, a very well-tolerated procedure. For some patients, you may need to add breast ultrasound for further testing. And for high-risk patients, a breast MRI can complement the mammogram.
Dr. Rachel Levenbach
If someone were to hand me a metal detector and say, “There is a 4 x 4 square-foot area with coins in the sand. Go find them.” Why would I not take the opportunity? This is one of those really low risk techniques – the exposure of radiation is very minimal. The yield with today’s 3D mammograms is so high that we’re finding more and more pre-cancers at a point where you can easily take care of them. So why would I not take the minimal harm for the maximum benefit?
Dr. Nandini Kulkarni
Preventing breast cancer
There are things we can do to prevent breast cancer. First, maintaining a healthy diet and a healthy weight has shown to decrease the incidence of post-menopausal breast cancer. And recent data has shown women who consume less than two alcoholic drinks per week have a lower incidence of breast cancer.
Dr. Kaitlyn Kennard
I always tell patients the importance of a healthy diet, and patients ask, “Well, what can I eat? Can I have a steak? Can I eat this? Can I eat that?” Usually whatever is good for the heart is good for the rest of the body as well. Ideally, plant-based diets are always great. And you’d be surprised how much decreasing the stress in your life can impact your health.
Dr. Yvonne Dansoa
Something that is often overlooked is exposure to extra estrogen. For post-menopausal symptoms, I find the go-to is still estrogen replacement. And while there’s absolutely nothing wrong with some baseline replacement – as long as it’s being monitored – I’ve had far too many patients who told me they were taking it for the last 15, 20 years. That is another major risk factor that patients can easily avoid.
Dr. Nandini Kulkarni
By getting screening mammograms, not only can you prevent it, but you can also pick up breast cancer at an early stage. We’re able to pick up either atypical cells that may in the future lead to breast cancer or pick up an extremely early stage, where very minimal treatment is needed. There are ways to catch it really early or prevent it from occurring.
Dr. Rachel Levenbach
A very important focus is identifying women who do not have breast cancer but are at increased risk for developing breast cancer. Some of those women are diagnosed with high-risk breast lesions – so they do not have breast cancer, but they do have high-risk lesions. Those patients usually are counseled in our high-risk clinic, where they meet with a breast surgeon and a medical oncologist. They are also eligible for increased imaging studies with a breast MRI on an annual basis, in addition to their mammogram. We talk to patients who fall in this category about some anti-estrogen tablets. Those tablets are usually offered for a period of five years, and they can decrease the chances of developing breast cancer by at least 50%.
Dr. Kamel Abou Hussein
For people who do have a known family history of breast cancer, we recommend a risk assessment and potential genetic testing. But for the majority of people, there are lifestyle behaviors which can reduce the risk of breast cancer: avoid weight gain, exercise – 75 to 150 minutes a week – avoid excess alcohol and avoid smoking.
Dr. Erica Linden
A patient’s mental state during breast cancer treatment
Patients will say, “I want to see my son’s graduation. I want to see my grandson marry.” It’s important for them to verbalize that because immediately, they’ve imagined what things will look like after they’ve been treated. At some point in our conversation, I will say, “20, 30 years from now.” And they will think, oh the doctor said 30 years from now, so I can still live a full life. That has a powerful impact in their mind. It is extremely important to present the fact that most breast cancer patients are now surviving to pretty much their full lifespan.
Dr. Nandini Kulkarni
Some patients have very good control of their ability to have peace of mind and deal with this in a healthy way. They are focused, taking notes, asking extremely important questions, and I’m always impressed. But the majority of patients are being human beings like the rest of us. They are extremely overwhelmed. Patients should be able to sit down with a provider who accepts that this is how they are dealing with this problem. Hopefully they can get to a stage where they can be clear about the plan and better able to deal with their disease.
Dr. Kamel Abou Hussein
Research has shown that a positive attitude can affect how a patient responds to their treatment overall, not necessarily that the treatment will work better, but how they move through that treatment is better, and they have a better quality of life. It’s incredibly important to acknowledge and address any sort of psychological issues that might be going on.
Dr. James Crawford
I see patients at the very, very early stages, where they go from being blissfully unaware and just living their life to having a new cancer diagnosis. It’s really important for me to project to them that breast cancer is a very treatable disease. I’ll point to patients who I’ve been seeing 20, 30, 40 years out from their cancer diagnosis, and I’ll say, “That can be you.”
Dr. Nikki Ariaratnam
There are resources we can refer to if people are having difficulty coping, because ultimately, it is scary. You’re facing a potentially life-threatening diagnosis. But your mental state helps frame how you tolerate things and can make the experience less obnoxious and less intolerant. I don’t want anyone to think you can will yourself out of a cancer diagnosis, but I also don’t want people to be suffering and miserable every moment. Helping support a patient through this process is why I do the work I do.
Dr. Erica Linden
Most patients have a good support system, but patients like to put on a brave face and tell their support system they’re fine, when really inside, they’re struggling. If I think a patient is struggling, I tell them they should talk to an outside therapist. The nice part about our network is there are social workers who specifically deal with cancer patients, so the patient can talk to someone who is outside their immediate family and they can let it all out.
Dr. Rachel Levenbach
Breast cancer doesn’t happen in a vacuum. Life is happening, and life can be messy. There may be people who will be very supportive, and people who won’t. I suggest they really find those people who can help them get through this really tough time. I give them the number for our breast cancer team and let them know we’re here to help guide them through this journey.
Dr. Kaitlyn Kennard
The emotional state of patients definitely matters from the beginning. It’s important for patients to have a good social support. If you’re stressed and you’re home thinking about your cancer diagnosis, that impacts your quality of life, and your quality of life really matters while going through your cancer care.
Dr. Yvonne Dansoa
What patients have taught them
They have taught me that you can be a 30-year-old mother of three children, and you can walk into your first appointment with a big smile and say, “I’m going to do this.” They have taught me that you can be a 100-year-old patient and say, “I’ll live another 20 years.” Patients have taught me to smile through adversity. They’ve taught me there’s always hope.
Dr. Nandini Kulkarni
Breast cancer patients teach me every day. I have learned resilience. I have learned that people are a lot stronger than they think they are, that they’re able to cope with more than they knew they could.
Dr. Erica Linden
It’s fascinating to be with patients as they go through this process and to see how strong they are. They find a strength they did not know they had.
Dr. James Crawford
You learn not to sweat the small stuff. I think about what I go through in my daily life. I’m working, I have a family, and these patients have the same thing, plus they’re fighting breast cancer. They’re very brave. They’re very strong. They find strength because they have to, because they don’t have a choice. It’s very rewarding to see that.
Dr. Rachel Levenbach
My patients have taught me gratitude. They are always grateful to their care team, and they’re grateful for the gifts they have in their lives.
Dr. Nikki Ariaratnam
My breast cancer patients have taught me how incredibly strong women are. A lot of women start their breast cancer journey saying, “There’s no way I can do this,” but they do, and they do it wonderfully. I think breast cancer is something that brings out a whole new level most women didn’t even know they had.
Dr. Kaitlyn Kennard
I keep learning about how we are built as human beings. I see a lot of new patients every day – I could be in one room where a patient is having a total breakdown, and the patient in the next room has the ability to be focused and in a calm state. We all take stressful news in a different way. I’m grateful to witness women from the beginning of their journey and be with them until the end of treatment.
Dr. Kamel Abou Hussein
My patients have shown me that their cancer diagnosis doesn’t just impact them, but also their family members, because women don’t just care for themselves. I have patients who want to live longer to be able to see their grandkids grow up. They’ve taught me hope.
Dr. Yvonne Dansoa
—BONUS Q&A—
Chemo brain
A good portion of women do get what is called chemo brain, or mental fogginess, which can be a challenging side effect, and I don’t think it’s being discussed enough. Women report being unable to remember names, numbers, daily habits, daily activities, whether they have done that activity or not. Sometimes women report being unable to remember addresses or phone numbers. That becomes quite challenging, especially for women. I try to talk to them about the importance of organizing their space, their desk, avoiding any form of clutter, maybe putting some cues to keep track of everything. Neuropsychologists can also help.
Dr. Kamel Abou Hussein
Patients will say, “I have chemo brain.” It’s difficult because we’re not sure if it’s coming from the chemotherapy regimen, from the tumor itself or the physical and emotional stress that patients are going through. Patients may have a difficult time focusing, completing tasks, remembering things, and it may take them longer to complete things than in the past. It doesn’t happen for all patients. Oftentimes, most patients find this chemo brain goes away after their cancer treatment is over.
Dr. Yvonne Dansoa
Many of our patients describe that concentration and attention is affected by chemotherapy, like they read a sentence and have to reread it, reread it, and they’re forgetful. We don’t have a magic pill to fix that. We have strategies – getting good rest, exercising, getting more oxygen to the brain seems to help. It is an area of active research, and I’m hoping in my career, we have better things to recommend.
Dr. Erica Linden
Their message to the newly diagnosed
You can do this, and you will do this. Find a good support system and a good team of doctors that you feel comfortable with. This is a road bump. It’s a small portion of your life.
Dr. Rachel Levenbach
There is hope. There are treatments available, and we’re here to support you. There’s a whole huge cancer team – from your breast surgeons to your radiation oncologist to your medical oncologist – and we’re here to help you.
Dr. Yvonne Dansoa
We’re here for you. There is help available. I strongly recommend that you put together a care team of people you trust and connect with, and who have explained everything to you in a way that you understand and appreciate.
Dr. James Crawford
Take a deep breath, you’re going to get through this and we’re going to get through it together. A lot of women are concerned about how this diagnosis is going to affect their family members and their job. They have to know to take care of themselves first – put on their face mask first on the airplane – to get through this journey.
Dr. Kaitlyn Kennard
When you are meeting your new care team, ask questions over and over because we are here to make sure everyone is clear about their choices. And a recommendation that is dear to my heart is to keep an open mind when there is a clinical trial available, because this is how we drive the field forward, and this is how breast cancer treatment continues to improve.
Dr. Kamel Abou Hussein
We’re here to try and make every step easier. We’ve been around the block a long time, enough time to be able to see the improvements in breast cancer care. So what they may remember their grandmother or their mother going through is not the way breast cancer treatment is nowadays. Be hopeful for the future.
Dr. Nikki Ariaratnam
Breast cancer is not one disease. It’s multiple diseases and there is a ton of information that patients can get from multiple providers. But you won’t immediately know what to do with that information – you’re not a breast cancer doctor. So just breathe, and learn, and make decisions with people who you’re comfortable seeing and discussing the plan.
Dr. Erica Linden
This treatment is a journey, just like life, and this journey is going to have its ups and down. One promise I can make to my patients is that I will hold their hand through every step of that journey.
Dr. Nandini Kulkarni