You might think drug addicts only live in Camden – certainly not in Cherry Hill, Marlton or Moorestown. But you’re wrong. Dead wrong.
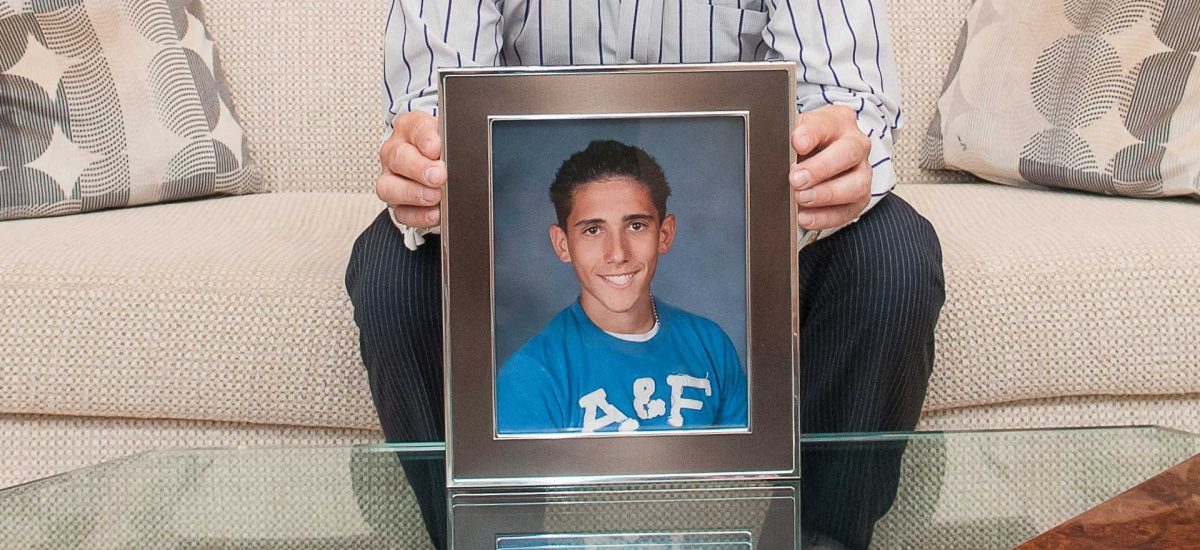
Gregg Wolfe didn’t know his 21-year-old son Justin was using heroin until the morning he died from an overdose in Wolfe’s Voorhees home. Like many young addicts, Justin hid it well until the very end, when the Temple University student was found unresponsive with four bags of the deadly powder stuffed in his jeans.
The 2009 graduate of Eastern High School seemed to have everything to live for at the time of his death. Beloved in his fraternity for his loyalty and compassionate nature, the gregarious young adult was keeping up his grades and, as far as his parents knew, had recently sought out treatment for a prescription medication addiction related to his struggles with anxiety, obsessive compulsive disorder and attention deficit hyperactivity disorder.
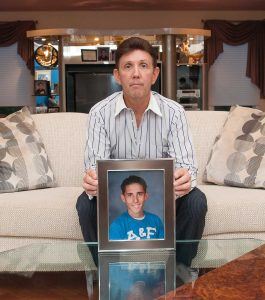
Gregg Wolfe lost his son Justin to a heroin overdose
“He was never happier in his life,” recalls Wolfe, president of a Philadelphia-based court-reporting firm. “Only after he passed away, when we looked back in his phone, we saw he had connections to sell his [medications]. From time to time, he was selling Adderall to make money, and he had pawned his computer and stole his mother’s jewelry to sell.
“Justin had a disease and, unfortunately, everybody missed it,” Wolfe continues. “It’s something an addict can hide very well. They can look in your face and tell you the sky is blue when it’s not.”
Once considered a dirty-needle, back-alley experience far removed from leafy suburban streets, heroin addiction has very quickly become “the number-one health care crisis” confronting the state, according to a 2014 report released by the Task Force on Heroin and Other Opiate Use by New Jersey’s Youth and Young Adults. This crisis affects countless young people once thought to be at low risk of addiction, notes the report from the Governor’s Council on Alcoholism and Drug Abuse. Moreover, the vast majority of addicts came to their dependency through prescription pain pills, sometimes legitimately acquired but also easily obtained on the black market.
As the task force put it, the line between legitimate medications and illicit street drugs has become blurred; “There is a disturbing new relationship between the doctor’s office, pharmacy and back-alley drug pusher.”
With the dubious distinction of being home to some of the most potent (and very cheap) heroin, South Jersey has been hit hard. Some 263 heroin-related overdoses have been logged in Camden City so far this year, including 22 fatalities, says Camden County Freeholder Director Louis Cappelli Jr. The death rate could have been far higher; 25 people were revived with the use of Naloxane, an antidote that can reverse an opiate overdose commonly used by many public safety and medical professions.
More telling, the vast majority of the users – 114 of them – were not city residents but suburbanites, mostly commuting from nearby communities to buy heroin.
Further proof that heroin addiction does not discriminate by zip code: Cherry Hill was listed among the top 20 towns in the state with the most documented heroin and opiate abuse earlier this year. The ranking was based on data provided by the New Jersey Department of Human Services.
“This is a problem that exists in every neighborhood, and everyone needs to be aware of it,” says Cappelli, noting that 80 to 90 percent of drug arrests in Camden City involve suburban users.
Beyond the horrific toll of young lives taken, heroin’s grip has led to an increase in crime throughout the region. Not only are the manufacturing, possession and selling of drugs a crime, but addiction also causes users to engage in risky and illegal behavior. In order to pay for their habit, heroin users often resort to theft, including break-ins in their own neighborhoods, the selling of family heirlooms and prostitution.
Activists like Gregg Wolfe are hopeful that more awareness of the complicating forces behind heroin’s spread will prevent some addictions and deaths. Squash the Secret, an advocacy group he founded, has been well received in recent months in its quest to speak to community and school groups. Yet there is much work ahead, he says.
“The amazing thing is that, even with the tremendous influx of heroin deaths all over South Jersey, people still look at people doing heroin and think they’re the scum of the earth,” he says. “They still don’t realize it’s a disease. The pull of the drug is so powerful. Addicts will lie, steal, do anything in order to get the drug.”

Heroin’s spread from slum to suburb involves several factors, from the significant increase in use of prescription painkillers to its low price in comparison to medically prescribed opiates, including OxyContin, Percocet, Percodan, Vicodin and Lorcet. Another factor that has changed the game is the potency of heroin sold on the streets. The drug is so pure that it can be crushed and snorted, or smoked, instead of injected intravenously. In the past, the need to shoot up into the veins was a deterrent that would turn off most recreational drug users from even trying heroin, according to experts.
Cherry Hill Police Lieutenant Amy Winters, commander of the department’s investigative unit, says heroin addicts interviewed after arrest typically have similar stories. They start with prescription pills, but when that habit becomes too expensive, they turn to heroin, which produces the high for $10 a bag verses $30 per pill.
“They just don’t correlate prescription pills, something they can get at a pharmacy, with how addictive it can become,” says Winters.
Moreover, she says, because pills are often easier to obtain than alcohol, and their effect less obvious to detect, teens often view opiates as a better alternative to drinking.
“They don’t have to worry about coming home smelling like alcohol or with it on their breath,” she says. “Pills are almost undetectable.”
Among the many chilling aspects of the heroin crisis is how quickly the use of medications commonly found in medicine cabinets can lead to a full-blown addiction, and then to heroin use, says Dr. Michael Shore, a Cherry Hill-based addictions specialist.
“Years ago, you wouldn’t really see most people with an alcohol addiction until they were in their mid to late 30s or 40s,” says Shore. “The progression now to [opiate] dependency happens so quickly. It can take a matter of a few weeks or a month or two.”
When people are prescribed opiates for physical pain, Shore explains, the medicine is tapered off when the pain improves, often with use of ibuprofen or similar medications for any residual pain. Physical dependency can occur with regular daily use of prescribed opiates in two weeks or less, depending on the frequency of use and dosage, and whether there is a predisposition to addiction in the family.
“When you’re hooked, if you stop using it, you’ll have withdrawal symptoms. You’ve developed a psychological dependency,” he says. In drug jargon, it’s called dope sick or dope flu.
“They might wake up one day after several hours of no opiate use thinking they have the flu: aches, pains, chills and sweats,” Shore explains. “Then someone will tell them, ‘You don’t have the flu. You’re dope sick.’”
Addiction will change the person’s brain chemistry. Sometimes this change takes months to fully resolve, but the change may be permanent, he says.
“This is a disease marked by relapse,” Shore adds. “As a chronic disease with no cure, it’s similar to other chronic diseases such as diabetes, hypertension and asthma that also have a longitudinal history of relapse. The drugs are calling your name, and effective ongoing management may include medication-assisted treatment, counseling and 12-step recovery meetings.”
While the state task force has identified many areas in need of reform, including more careful drug monitoring by physicians and the requirement that all insurance plans cover comprehensive treatment programs, there is also widespread agreement that awareness of opiate and heroin addiction is urgently needed.
To that end, in May, Camden County held a symposium titled “The Opiate and Heroin Crisis In Our Community,” which drew more than 700 people to discuss the issue with educators, law enforcement and treatment specialists. In addition, the county has also purchased four billboards with the slogan “Heroin. Pills. It All Kills.” Featuring a clean-cut white teenager, the signs include information on a hotline number and the additional message: “It’s not miles away. It’s not other kids. It’s right in your backyard.”
“This is something we as a county can’t stop or cure, but we can help our residents learn about the problem, hopefully prevent it and assist people in finding help,” says Cappelli.
Samost Jewish Family and Children’s Services, a social services agency, has taken a lead as both a sponsor of the symposium and by launching a new recovery addiction support group sponsored by Wolfe. The nonprofit organization also plans to offer drug addiction seminars to interested groups.
Wolfe, who founded the awareness group Squash the Secret after his son’s death, also speaks widely, both to lobby for reform of the HIPAA Law (the Health Insurance Portability and Accountability Act of 1996) and to urge parents to consider taking legal steps, including seeking Power of Attorney over their children, to gain control of their medical management. Currently, the HIPAA Law protects the medical records of young adults over 16 in New Jersey. In Justin’s case, at least two of his doctors were aware of his heroin use, but under the law, his father was not entitled to know.
In Cherry Hill, the crisis has brought together the police department, schools and municipal government to pool together resources, share information and update curricula. Wolfe spoke to seniors at Cherry Hill East and West High Schools and the Zone PTA, comprised of the PTA presidents of every district school. Moreover, a Kennedy University Hospital representative lectured juniors about the dangers of prescription drugs, says Linda Dombrowski, director of Schools and Communities Organized for Parent Education.
Students learn in health classes about New Jersey’s recently approved Good Samaritan Law, which allows a person to call police to report an overdose without fear of repercussion, says Jennifer DiStefano, student assistance counselor at Cherry Hill East. There is also discussion about the drug trade.
“We tell them that drug suppliers are there to make money and students, as buyers, are getting the short end of the stick,” she says. “They won’t be there when you’re down and out and struggling with addiction.”
Perhaps harder to reach are parents and even grandparents, many of whom are still unaware that their drug supplies should be locked up. Much like earlier generations raided their parents’ liquor cabinets, some teens are taking pills from their family medicine cabinets, says DiStefano.
“It’s important to educate everyone that when they go to the doctor for a backache and get Percocet or OxyContin, they probably don’t realize they haven’t taken the full prescription and throw it back into the medicine cabinet,” she says. “Kids are looking for these things. They might not be using them, but they could be selling them to make money.”
Meanwhile, Wolfe’s advocacy group has a roster of recovered addicts and parents who’ve lost their children to heroin and who are willing and eager to tell their stories to any and all groups.
Among members, Voorhees resident Sue D’Ambrosio is a frequent speaker. The story of her son Mark, a bright young man who loved baseball as a kid, speaks to many parents who could never imagine their child succumbing to heroin addiction as Mark did the summer before college. In treatment, Mark realized he had a disease and tried desperately to fight it, says his mom. But in the end, he died of an overdose in December 2009.
“Parents think it won’t happen to their children because they’re into sports and close to their family, but so was mine,” says D’Ambrosio, who self-published the book “Why My Son?” detailing the family’s journey. “He was a church-going Catholic, which was how I was raised. My father was a family physician, and even he couldn’t save Mark’s life.
“We tried everything: counselors, meetings, in-patient treatment, outpatient crisis centers, arrest,” she adds. “I don’t think there was anything more we could have done. I’m at peace. I tried everything, and now I’m trying to help others.”