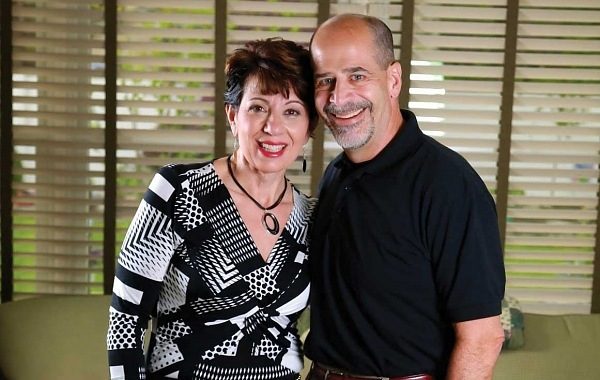
For many, surgery can help shed pounds Bob Alesiani and Claire Masino-Alesiani have shared much in their 34-year marriage – a home, a son and their ongoing weight struggles. What separates the two are their reasons for getting bariatric surgery almost five years ago.

Claire and Bob Alesiani before
Bob was dismayed about his skyrocketing blood pressure and cholesterol. The 290 pounds he was carrying also took a toll on his joints, culminating in a double hip replacement before he turned 50. The final straw was being diagnosed with diabetes.
“It was all about the numbers – the blood pressure and cholesterol. These were the numbers I wanted to change. The weight was secondary to the health outcome,” says Bob, who has lost 110 pounds since his laparoscopic gastric bypass in 2009. “My family loves me, heavy or thin. Now it’s easier to buy clothes, but there were health reasons.”
The numbers from every medical test mattered to Claire also, but she sought surgery because she was tired of being tired. A combination of sleep apnea, asthma and acid reflux so intense she had to sleep sitting up was dragging her down. Her weight, which is 125 pounds less since her laparoscopic gastric bypass performed a week before her husband’s, complicated her everyday life.
“I wasn’t looking for a bikini body. I wanted to feel better and fit into clothes and plane seats,” says Claire, who, true to her number-less outlook, declined to give her pre-surgery weight but says she has a “very healthy BMI.”

and after undergoing weight-loss surgery
With their adult son’s bariatric surgery as inspiration, Bob, who was 51 at the time, and Claire, then 50, followed suit. The Lumberton couple agreed to put aside the trendy diets they had tried on and off for years and scheduled their surgeries days apart so they could support each other in the aftermath.
“I couldn’t see not doing it together; we had the same issue,” says Claire.
“I was taking nine medications a day, and they were getting ready to add two more,” says Bob. “It got to the point where there were not many options left.”
Bariatric surgery is the last stop for many people, Bob and Claire included. Just as there are choices of diets, several weight-loss surgical options exist – and picking one is just the start. It is a journey doctors say almost anyone can do as long as they are committed to what comes before and after surgery.
More than a third of adults in the United States are obese, and almost a quarter of New Jersey residents also meet the criteria for obesity (BMI of 30 or greater), according to the Centers for Disease Control and Prevention. But those numbers don’t mean people have given up the battle – and surgery is one of the most serious weapons in the arsenal.
Prospective patients can choose from two surgical categories: restrictive, which reduces stomach size; and malabsorptive/ restrictive, which reduces stomach size but also removes or bypasses some of the digestive tract.
Possibly the most widely known restrictive surgery is adjustable gastric banding, which divides the stomach by using an inflatable band. Another option – vertical banded gastroplasty – uses staples and a band to reduce stomach size, while sleeve gastrectomy removes 75 percent of the stomach and leaves a passageway that connects to the intestines. The new kid on the block is gastric plication, which involves sewing folds in the stomach to reduce its size.
Gastric bypass is the most well-known of the malabsorptive/restrictive procedures. During the procedure, the stomach is divided, and the smaller upper portion is connected to the intestines. In another, more extreme version of the gastric bypass, a majority of the stomach is removed and what is left bypasses much of the intestines.
“The adjustable band and gastric bypass used to be the only choices. What we have now has been built upon through years of operations,” says Lisa Medvetz, MD, director of the bariatric and meta-bolic surgery program at Lourdes Medical Center of Burlington County. Medvetz says she recommends her patients choose what procedure is best for them.
Choosing a surgery requires more than skimming a brochure. Patients must consider any other health issues, as well as how much weight they have to lose. To start, patients must have a BMI of 40 or more, or a lower BMI with other troubles, such as heart disease, to be considered for weight-loss surgery. Surgeon Samuel Wasser, MD, says most of his bariatric patients are between 20 and 50 years old, but some in their 60s and 70s also want the surgery.
“I’ve done surgery on patients up to age 72. If your heart and lungs are fine, then you are a candidate,” says Wasser, who specializes in bariatric surgery at Virtua. “The best candidate is anyone who is motivated.”
Medvetz, who agrees dedication determines post-surgery success, finds more women than men come through her doors. She has a 90/10 split, she says.
“For women, the goal is not to be in a bikini, but to have energy,” says Medvetz. “Women are also critical of themselves. There is a lot of discrimination against obese people, and women pay more attention to that discrimination.”
Some factors can rule out a patient, no matter the gender, such as severe weight gain or drug abuse in the months leading up to surgery. Patients must undergo physical and mental screenings to show if they’re ready for surgery – or not.
“It’s not just being physically there, but mentally there,” says Medvetz. “It shows you really want it and you will be motivated to change your lifestyle.”
In fact, the process begins with medical exams and a psychological evaluation, which includes questionnaires on eating behaviors and mental state. The assessment, says Dina Goldstein Silverman, PhD, begins with the first interview.
“It’s not just one interaction. It’s a snapshot of a million components that contribute to an overall profile,” says Silverman, psychologist for the Cooper University Health Care Center for Metabolic and Bariatric Surgery. “They are being asked to make big changes to their life. If they are not ready to do that, we will work with them.”
Silverman digs deep to uncover a patient’s relationship to food, as well as why and when they eat. Food, she says, has many meanings. It can be social, familial or comforting.
“There are those who pour a drink, light a joint or call a friend. Some will have a cookie. They are not hungry, but they are self-soothing,” says Silverman. “If they grew up poor and there was not a lot of food or they were the youngest with not much food, they may overeat at a meal. They may have a history of trauma or sexual abuse. What is that part of their history? There’s something behind their battle and their underlying emotions and thoughts.”
Just as all surgeries have a screening process, they all have risks and benefits. Depending on the type of bariatric surgery selected, risks can include hypoglycemia, gallstones, hernias and ulcers. Eating too much sugary or carb-heavy foods can lead to “dumping,” which causes sweating, vomiting and diarrhea. While any surgery carries a risk of death, that risk is less than 1 percent for all bariatric procedures, according to the American Medical Association.
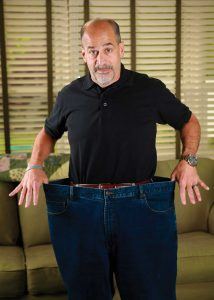
Bob Alesiani has lost 110 pounds since undergoing weight-loss surgery
Clearly, significant weight loss is the most obvious benefit of these surgeries. With it, there can be higher self-esteem and confidence. Silverman has seen depression abate due to the lessening of physical pain and increased exercise. The mindful eating techniques taught prior to surgery, which aid in breaking long-held habits, also improve coping skills, she says. For women, says Medvetz, weight loss can also be a boon to fertility.
“Then there’s the medication costs – you are no longer paying for medicines for diabetes or for an apnea machine,” says Wasser.
Bariatric surgery patients must dramatically change their lifestyle – especially their diet. They begin drinking only liquids then advance to pureed foods and soft solids before settling into small portions of solid foods. The process takes months, and doctors and nutritionists follow patients closely. Support groups allow patients to share stories and experiences.
“We continue to go to the support group because it reminds us of what we did and why we did it,” says Bob Alesiani, “so we never fall too far behind.”
He and wife Claire say they are doing well physically and mentally. Claire’s asthma and sleep apnea are gone, and her reflux is under control. Bob no longer takes medication for his arthritis. He plays lacrosse, which he hasn’t done since college, and Claire takes a dance class, which has always been on her bucket list. Both know surgery was not the end, but instead the beginning of a new fight in their ongoing struggle.
“The pounds of pasta from before are long gone. Now it’s proteins, fruits and vegetables,” says Claire. “It’s more difficult now than in the past five years. It’s thinking about it every day.”